Michael Drummond
Feb 21, 2021

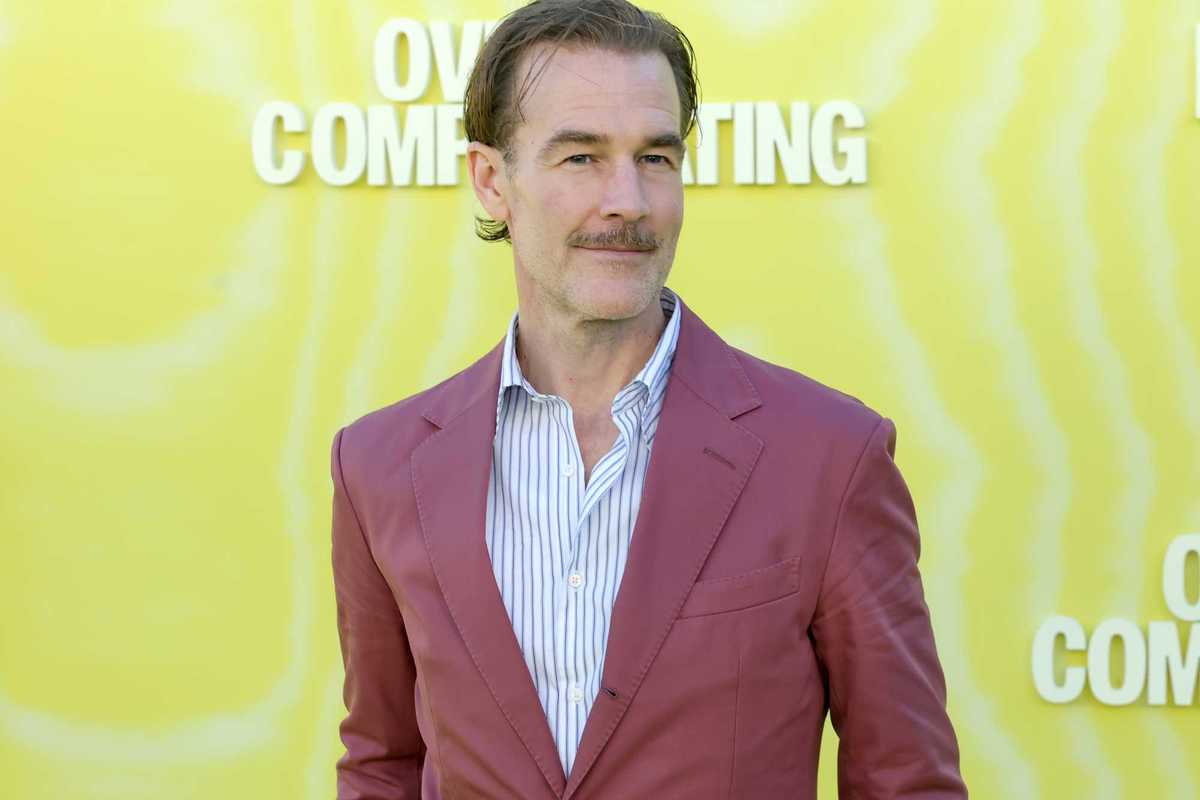
Transplant patient Anna Hadley outside Great Ormond Street Hospital
NHS doctors have become the first in the world to give children new hearts which have been brought back to life by a ground-breaking machine.
Staff at Great Ormond Street Hospital (Gosh) and Royal Papworth Hospital (RPH) collaborated on the medical breakthrough, which saved the lives of six youngsters in 2020.
The “game-changing” technique – known as donation after circulatory death (DCD) – sees hearts being reanimated and kept beating outside a human body until they are ready for transplanting.
Donated hearts have historically come from people who are brain-dead but whose hearts are still beating, which limits the scope for the number of transplants possible.
DCD not only allows more hearts to be used, it also allows them to be transported further and gives surgeons and nurses more time.
The ground-breaking technique was first performed in Europe at the RPH in 2015 but has until recently only been possible in adults.
The collaboration between RPH in Cambridge – whose team retrieves the heart – and Gosh, whose team implants the organ, as well as NHS Blood & Transplant, represents the first-ever use of the DCD technique in paediatric transplantation anywhere in the world.
Jacob Simmonds, consultant cardiologist and transplant physician at Gosh, hailed the significance of the programme.
He said: “In early 2020 we had more children at Gosh on the transplant list than I’d ever seen in my 16 years working at the hospital.
“Every day a child waits there is a bigger likelihood that they may get too ill even for transplantation, or worse.
“Although medical advances have come far, for some children with heart failure an organ donation is truly their only hope.”
The DCD heart programme has unlocked more opportunities for donation, essentially doubling the number of transplants done at Gosh in eligible patients weighing more than 44lb (20kg), he said.
“It’s game-changing and work is already under way to make the technique suitable for our much younger and smaller patients.
“Ultimately, though, this still relies on families having conversations around their organ donation wishes, and then of course the bravery to consider making this precious, life-saving gift at a time of unimaginable tragedy.”
The first patient to receive a DCD heart thanks to the partnership was 15-year-old Anna Hadley.
Anna was diagnosed with restrictive cardiomyopathy after collapsing during a PE class two months earlier.
The rare condition meant that the muscles in the lower chambers of her heart – the ventricles – were becoming stiff and could not fill with blood properly, which affected the blood flow to the rest of her body and heart.
After an assessment at Gosh, the family were told that Anna’s best chance of getting well again was a heart transplant.
Her father, Andrew, said: “After weighing up the potential risks and benefits of the DCD heart transplant with a more conventional one, we realised that there was only one choice, and we’re so glad we made it.
“Five days after the transplant, Anna was walking up and down the corridors, chatting away and high-fiving staff. It was incredible.”
Across Britain there is a shortage of suitable donors, which means that the number of children who would benefit from organ transplantation exceeds the number of organs available.
Children face longer-than-average waiting times due to the difficulty of finding the right match and because the consent rate for paediatric organ donation is much lower than the national average for adults.
Marius Berman, consultant cardiothoracic transplant surgeon at the Royal Papworth Hospital, said: “No-one else in the world is currently doing this.
“It’s been an incredible multi-institutional and multidisciplinary team effort to make this possible, involving everyone from the specialist nurses in organ donation and retrieval, transplant co-ordinators, physicians and surgeons.
“Above all, none of this would be possible without the generosity of every donor and their families.”
Top 100
The Conversation (0)