The only reason I know about diabulimia is because it happened to a friend.
Natalie Holborow, a poet and writer who lives in Swansea, Wales, suffered from diabulimia when she was 22-years-old, but has since recovered and managed to reverse the damage caused by the disorder.
She wrote a Facebook post reflecting on her recovery and her condition when she was suffering from diabulimia:
I was severely underweight, terribly affected by the bullying I went through in school and cut back on insulin, something which is life-threatening as a Type 1 diabetic. I was so far into my illness it was impossible to think rationally. I was blue with cold a lot of the time, losing my hair, hormones didn’t work and you can see in my eyes how sad and consumed by it I was.
Remembering how Natalie was then – shivering within five minutes of a night out, and me feeling that I might break her whenever we hugged - compared to who she is today – a fiercely independent, strong-willed woman who just completed a Tough Mudder half – is reason enough to want to raise awareness of a disorder so few people seem to have heard of.
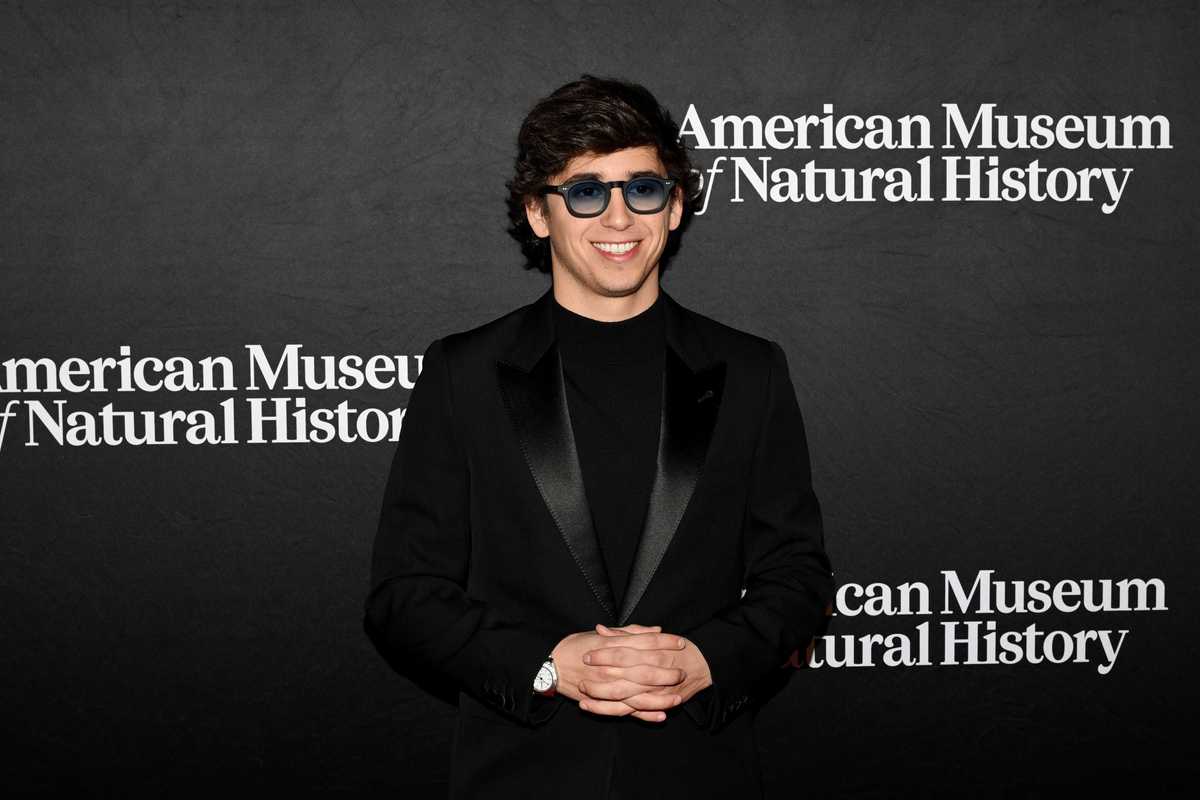
Natalie aged 22, and now, in 2016, aged 25
Diabulimia is viewed by experts, such as the charity b-eat, as an eating disorder that sees people with Type 1 diabetes deliberately take less insulin than they need, with the intention of losing weight. It is not yet a recognised medical condition and there have been several calls by charities to change that.
A spokesperson for b-eat told indy100:
At the moment diabulimia is not yet recognised as a medical condition, more a behaviour around eating. Eating disorders are serious mental illnesses and this type of behaviour could possibly lead to the outcome of a diabetic developing an eating disorder.
Research suggests that 40 per cent of women with Type 1 diabetes between the ages of 15 and 40 have, at some point, restricted their insulin to control their weight.
As Natalie writes in her Facebook post, other sufferers aren’t as lucky as her.
In April The Telegraph reported the case of Lisa Day, who was 14 when she was diagnosed with Type 1 diabetes. Her weight plummeted, and she was also diagnosed with anorexia.
She was seen by a psychiatrist at an eating disorder clinic, but little was known there about diabetics, so they concentrated on her issues with food – not insulin.
Her family believe that when she was 27, she stopped taking overly low doses of insulin, but by then it was too late. She had serious health problems including kidney damage and severe eye disease.
She died on 12 September 2015.
Jacquelin Allan, founder of the charity Diabetics With Eating Disorders DWED, told indy100 that it is not unheard of for people with diabulimia to be put in eating disorder wards with no insulin.
This has happened because what we need to treat diabulimia is a well-connected multidisciplinary team.
A diabetes team to educate the ED (eating disorder) team and vice versa. In reality this is incredibly rare. The patient gets placed in a ward that may have never treated a Type 1 before, with staff who may not medically trained and therefore have no understanding of what they are actually looking at.
Without insulin a Type 1 will eventually fall into a condition called Diabetic Ketoacidosis which is always fatal without speedy treatment. The whole point of going into treatment is to keep you safe as you mentally can't be responsible for your diabetes treatment. But I have known many people who quite honestly would have been safer with their families or anyone who had even a rudimentary understanding of Type 1.
She explained that the entire situation of diagnosing and treating diabulimia is incredibly complicated. Although diabulimia is not a recognised medical condition, the omission or manipulation of insulin specifically for weight control is a clinical feature of both bulimia and anorexia.
So you may ask yourself: what is the difference between these diagnoses for a Type 1 diabetic who omits insulin?
The answer is weight. For example two Type 1 's with identical eating disorder behaviour but different weights will be diagnosed with different eating disorders.
This is problematic for a number of reasons, while weight might be the biggest risk factor in a standard ED, in Type 1 a more accurate risk measurement is HbA1c (average blood sugar over 3 months). The resulting situation is Type 1s who are gravely ill who can't get treatment because their weight isn't low enough.
Diabulimia has been blamed by some in the medical profession on a lack of knowledge and instruction for those with diabetes, but Ms Allan says this is “absolute nonsense”.
Diabulimia is a mental illness, similar in psychology to anorexia or bulimia, but also with diabetes specific psychsocial issues,
In fact most people with diabulimia also exhibit more classic symptoms such as fasting and/or purging.
I know people who have fallen pregnant when diabulimic and in a bid to protect the child attained perfect blood sugar within a matter of days, if it was an issue of education this couldn't happen.
Some people may not take their insulin properly out of ignorance but the chronic long term under-dosing of insulin for weight loss purposes is a mental illness, not a lack of knowledge, or a phase, or a rebellion or a cry for attention.
A new set of guidelines for the treatment of eating disorders, which includes how best to treat those who also have diabetes, is expected to be released by the National Institute of Health and Care Excellence (Nice) in early 2017.
A spokesperson for the NHS told indy100:
We are clear in our ambition to join up care for mental and physical health so that patients have all of their needs met holistically.
We know that people with long term health conditions such as diabetes are also more likely to suffer from mental health problems and to try and tackle this, NHS England has committed to integrating psychological services with physical health, including deploying 3,000 new mental health therapists to GP practices.
We are also investing 150 million to ensure children and young people with eating disorders get access to treatment as quickly as possible.
'It's OK to speak out about it,' Natalie says.
Health professionals really need to keep an eye on patients to recognise that what they often deem to be 'rebellion against diabetes' could in fact be an eating disorder. You can clearly see the difference in weight in the two pictures but the biggest difference? My smile. I'm fully living life now.
Diabetes is not just physical, and more needs to be done to support people mentally. Health service needs to wake up to the fact that with diabetes being so focused on food and control, more support is needed not to make patients feel guilty for bad blood sugar levels but to realise it may be a cry for help.
More: Six little-known signs of stress
More: This is the secret to being happy according to psychiatrists